CAREGIVER PROTOCOLS
for
In-Home Care
Developed in the Context of the Public Health Emergency Related to COVID-19 by Family Member for other Family Members*
*This document (prepared and printed as of April 22, 2020) was developed in the context of the public health emergency related to COVID-19 (SARS-CoV-2) specifically for the purpose of assisting caregivers and family members responsible for their loved ones in their home.
Medical literature, state/national guidelines, and expert consensus continue to evolve relative to COVID-19. The caregiver protocols and related information herein are based on current knowledge gained through consultation with experts, medical professionals, online research, and an awareness of the limited availability of PPE (e.g., masks). This document is a response by the family to its critically urgent need to provide practical guidance to the Client’s in-home caregivers in order to mitigate the risk of infection from and spread of SARS-CoV-2. This document was not prepared by medical professionals. It was prepared by concerned family members of a Client. It is not meant to replace, substitute for, or overrule a qualified medical professional’s judgment and it is not meant to substitute for the practice of medicine or the provision of any medical professional services.
Overview
COVID-19 is the disease caused by a virus named SARS-CoV-2.
What Can I Do to Protect Myself, Clients, and Others?
The most important thing you can do to protect yourself, clients and others are to practice good hygiene:
- Handwashing, handwashing, handwashing
- Do not touch your face before washing hands
- Practice social distancing of 6 feet to 10 feet
- Wear a mask when assisting clients or if within 10 feet of a client
- Wear gloves for food preparation or when assisting with medicine or hygiene-related activities such as bathing, toileting, etc.
Does the Risk of Death from COVID-19 Increase with Age?
Older people, especially those with health issues have a higher risk of dying when compared to those who are young and healthy. Statistics change daily but recent studies done by the U.S. Center for Disease Control (CDC) indicate approximately 91% of those who have died were age 55 or older and 78% were age 65 or older.
How is SARS-CoV-2 Transmitted from Person to Person?
Much is still unknown about the transmission of the SARS-CoV-2 virus. However, a person with COVID-19 may not “appear” sick and may not feel sick. Yet, a cough, sneeze, or even a breath from an infected person will emit infectious virus particles into the air (aerosols) that can be inhaled and potentially infect another person. Public health experts have generally recommended maintaining social distance of 6 feet to reduce the chance of inhaling infectious aerosols emitted from another person. Some studies have recommended maintaining a social distance of 10 feet due because aerosols emitted from sneezes or coughs can travel further than six feet.
Sneezing/coughing into a hand or touching a runny nose and then using that same hand to touch a person or an object (e.g., a doorknob or virtually any surface or object) can leave behind infectious SARS-CoV-2 virus that has the potential to infect another person.
Why is Handwashing and Wearing a Mask Important?
Frequent handwashing and the use of facemasks (and gloves) reduces the risk of infection from the SARS-CoV-2 virus. The importance of adopting these practices cannot be overstated.
Masks reduce the likelihood of inhaling infectious aerosols as well as the risk of spreading infectious aerosols if the wearer is infected.
Washing hands and proper use of gloves reduces the likelihood of becoming infected if exposed to SARS-CoV-2 as a result of touching an infected person or a contaminated surface or object. It also reduces the likelihood of transmitting the virus to others.
SARS-CoV-2 virus can live in the air and on surfaces as follows:
- Up to 3 hours in the air (aerosols)
- Up to 72 hours (3 days) on stainless steel and plastic surfaces/objects (e.g., countertops, TV remote controls, etc.)
- Up to 24 hours (1 day) on cardboard (e.g., Amazon boxes, egg cartons, etc.)
Are Caregiver Protocols Mandatory?
Caregiver Protocols are mandatory in all situations. They are extremely important and represent a “best practice” based on our current knowledge. These protocols should be followed in the normal course of caregiving. However, in the normal course of caregiving unique and challenging situations may arise making it difficult or impractical to follow a protocol and, as such, a caregiver may conclude it is safer to perform an activity in a manner other than what is prescribed by these protocols. In these instances, professional judgment, awareness, an informed understanding of how to limit the spread of infection and knowledge of the practical limitations of using personal protective equipment should be carefully considered. And, we ask that the caregiver document the facts and circumstances along with reasons for the actions taken. This documentation will help everyone on our team continue to learn, adapt, and develop new protocols for addressing unique and/or unforeseen situations.
In all situations please remember the importance of handwashing, handwashing, handwashing…and the need to wear a mask within 10 feet of the Client and other family members.
COVID-19 CAREGIVER PROTOCOLS
To protect yourself, clients and others and to limit the spread of SARS-CoV-2 the following protocols should be followed upon entering the premises and/or when caring for:
Arrival
- Take temperature before arrival (no entry if 99.0+)
- Clean clothes required (or use disposable gown)
- Wash hands upon entering home (see attached handwashing guidelines)
- Fingernails must be clean
- No rings or watches (minimal jewelry)
- Arrive without makeup and hair worn up or in a hairnet
- Disinfect personal items such as cell phone, etc. (please leave nonessential personal items in the car)
Masks
- Use best mask available (N95 respirator, surgical facemask or cloth mask)
- Must be worn in the client’s room (whether or not the client is present)
- Must be worn within 10 feet of a client outside his/her room
- Must be worn when preparing and serving food, medicine, etc.
- Must be worn if other people are in the home (family, other caregivers)
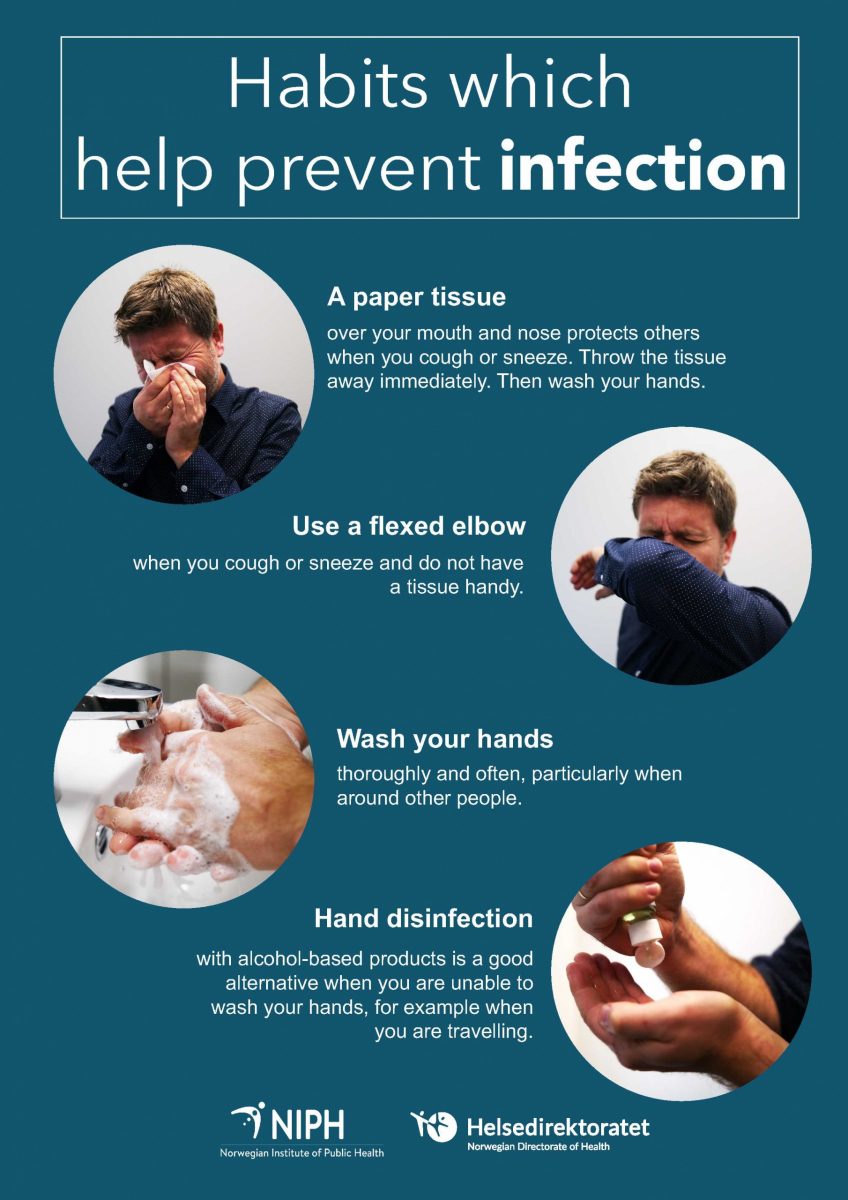
Respiratory Hygiene and Cough Etiquette
When not wearing a mask, respiratory hygiene and cough etiquette must be followed:
- Cover mouth and nose with your bent elbow or a tissue when coughing or sneezing. Dispose of the used tissue immediately.
- Wipe surrounding areas if possibility mouth/nose not properly covered
- Wash hands immediately afterward
Gloves
- Gloves do not replace the need for frequent handwashing
- Gloves must be used for the following activities
- Food preparation and serving food
- Handling and delivery of medicines
- Assisting with hygiene-related activities such as toileting
- The use of gloves is mandatory if the caregiver has cuts, open wounds, or bleeding.
- Discard gloves after each use and immediately wash hands
- Use of gloves in situations not listed above is not mandatory and the decision is left to the professional judgment of caregivers
During and at End of Shift
- Wash hands regularly during your shift and always after performing activities listed in the HANDWASHING attachment.
- Practice respiratory hygiene and cough etiquette as explained above
- Avoid unnecessary touching of the face
- Wash hands before touching Client’s face or hair
- Bleach, alcohol, hydrogen peroxide, or ammonia-based disinfectants should be used to disinfect surfaces when cleaning. If uncertain about the product being used please reference the following website:
- Kitchen and Laundry Areas
- Clean kitchen surfaces and countertops with a disinfectant
- Disinfect refrigerator handles, faucet handles, stove controls, etc.
- Disinfect washer and dryer handles
- Disinfect door handles
- Wash kitchen towels and Client’s towels/clothes as required (launder with “hot” water setting)
- Accumulated trash should be discarded in outside trash bin
- Cleaning Client’s Room and common living space:
- Disinfect horizontal surfaces (tabletops, etc.), fixtures and commonly used objects such as the following:
- Phones, earbuds, tv remote, eyeglasses & other commonly used items
- Change towels on the recliner chair
- Disinfect caregiver binder cover
- Accumulated trash should be discarded in outside trash bin
- Cleaning Client’ restroom:
- Clean and disinfect toilet
- Clean and disinfect doorknobs, drawer pull handles, light switches and commonly used bathroom items
- Clean bathroom countertops and other horizontal surfaces
- Accumulated trash should be discarded in outside trash bin
Personal Protective Equipment (PPE)
- PPE is in short supply – use the best equipment available
- An N95 respirator/mask is preferable to a surgical mask
- A surgical mask is preferable to a homemade cloth mask
- A homemade cloth mask is better than no mask at all
- Exhale vents on disposable masks (respirators) should be sealed shut to prevent the wearer from spreading aerosols.
- Do not reuse disposable surgical gowns if it becomes soiled or wet.
- Masks should not be shared among caregivers!
- Masks should not be washed, wiped down, bleached, or sprayed with alcohol. These disinfection methods will degrade the fabric and compromise the ability of the mask to protect against inhaling the SARS-CoV2 virus.
- Homemade cloth face coverings should be washed after each shift.
- Disposable masks are (generally) not tested or approved for disinfection and reuse. Nonetheless, recent research studies have identified viable disinfection methods to be used as a crisis strategy during this pandemic when masks are in short supply.
- No disinfection strategy is currently available for single-use surgical masks (as of 4/18/20)
- No disinfection or reuse strategy can be recommended at this time. Nonetheless, at the end of a shift, masks should be placed in a breathable paper bag and the caregiver should write their name and the date of last use on the outside of the bag. Absent an alternative disinfection strategy, a caregiver should, if possible, wait at least five days before reusing a mask.
- N95 masks with an exhale vent MUST have the vent sealed shut (with tape, etc.) prior to use. Generally, masks with exhale vents are not appropriate when caring for clients because they protect only the caregiver. However, due to a shortage of masks, these masks may be used if the exhale vent is sealed shut.
- Any N95 or KN95 disposable masks may not be disinfected at this time.
HANDWASHING: Key Times to Wash Hands
Help yourself, your loved ones and your clients stay healthy by washing your hands often, especially during these key times when you are likely to get and spread germs:
- Before, during, and after preparing food
- Before eating food
- Before and after caring for someone at home who is sick with vomiting or diarrhea
- Before and after treating a cut or wound
- After using the toilet
- After cleaning up someone who has used the toilet
- After blowing your nose, coughing, or sneezing
- After touching an animal, animal feed, or animal waste
- After handling pet food or pet treats
- After touching garbage
During the COVID-19 pandemic, you should also clean hands:
- After you have been in a public place and touched an item or surface that may be frequently touched by other people, such as door handles, tables, gas pumps, shopping carts, or electronic cashier registers/screens, etc.
- Before touching your eyes, nose, or mouth because that’s how germs enter our bodies.